Health System Redesign First-Year Implementation Plan February, 2008 - March, 2009 | |
Background | |
In February, 2008, the San Mateo County Health System Redesign Initiative (Redesign) was created to address both the financial sustainability and system and policy opportunities for the healthcare delivery system for uninsured and underserved populations. The Redesign aims to accomplish the following charge: | |
Within two years, design and implement a new, sustainable and creative approach to healthcare delivery that incorporates key recommendations of the HMA Phase 2 Final Report and the recommendations of the Blue Ribbon Task Force on Adult Health Care Coverage Expansion. | |
Led by the County Manager, this initiative’s core staff team includes: Sang-ick Chang, CEO, San Mateo Medical Center (SMMC); Susan Ehrlich, Interim Chief Medical Officer, San Mateo Medical Center; Charlene Silva, Director, San Mateo County Health Department (HD); Maya Altman, Executive Director, Health Plan of San Mateo (HPSM); and Srija Srinivasan, Special Assistant to the County Manager for the Redesign Initiative. | |
This document outlines the first-year implementation plan for Redesign, including seven areas of priority focus, targeted goals for each of these areas, priority activities, and next steps in designing an evaluation plan that will address cross-cutting efforts that encapsulate Redesign’s targeted impacts. | |
Discussion | |
Redesign team members reviewed the Blue Ribbon Task Force’s (BRTF) deliberations and analysis aimed at identifying local delivery system capacity to meet the needs of the uninsured and underserved. The Health Management Associates (HMA) Assessment of Strategic Priorities for San Mateo Health Services, which was accepted by the Board of Supervisors on February 5, 2008, complemented the work of the BRTF and provided detailed findings and recommendations regarding: a) the County’s Healthcare Role within the Broader Community; b) Medical Services Delivered by the San Mateo Medical Center; c) the County’s Psychiatric and Long Term Care services; d) the Health Plan of San Mateo; and e) Financial Capacity and Opportunities for the healthcare delivery system. | |
From these sources of information, the Redesign team members identified the following seven areas for priority focus: | |
1) |
Physician Leadership, Structures, and Accountability; |
2) |
Chronic Disease Management and Care Coordination; |
3) |
Integration Across Levels of Care; |
4) |
Physician Leadership, Structures, and Accountability; |
5) |
Community Health Network for the Underserved; |
6) |
Long-Term Care; and |
7) |
Strategic and Operational Financial Improvement. |
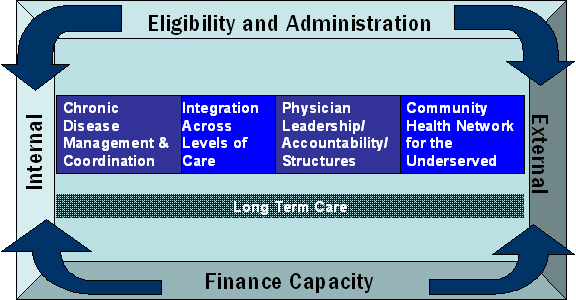
The factors guiding the selection of the above priorities included an assessment of areas of greatest potential impact in meeting County mission and responsibilities and improving the County’s financial position in delivering healthcare to underserved populations. In addition, Redesign team members considered the way in which the County intersects with and plays a part in the broader local healthcare delivery landscape. Across these areas, there are both internal (i.e., within and across County systems) and external (i.e., with private healthcare providers) opportunities for improved effectiveness and efficiency. The following diagram displays the alignment of these priorities across the internal/external continuum. | |
| |
The following goals and first-year actions, by priority area, address the client, system and financial outcomes targeted by the Redesign Team. | |
Eligibility and Administration | |
Overall Goals: | |
● |
Maximized enrollment of, and retention in, public health insurance/ coverage programs with emphasis, in the first year, on Medi-Cal |
● |
Streamlined administration of public insurance/ coverage programs for the underserved |
Key First-Year Actions: | |
1. |
Appoint cross-system (SMMC, HPSM, HD, Human Services Agency (HSA)) workgroup with accountability to HPSM Executive Director and HSA Director. |
2. |
Identify gaps and problems with current eligibility, enrollment and retention (EER) processes from a client- and systems- point of view. |
3. |
Recommend an organizational structure for optimizing EER and minimizing administrative costs with clear accountability for: a) operational leadership and day-to-day decision-making; b) defined roles for each County entity; c) effective liaison to non-County entities (e.g., Social Security Administration, Private vendors, other); d) policy oversight and decision-making. |
4. |
Select and complete at least two initiatives for increased enrollment and retention of public insurance/coverage programs, with emphasis on Medi-Cal. |
5. |
Develop proposal and obtain needed agreement by governance/ policy boards to transfer administration of indigent care programs to HPSM in order to implement a seamless and coordinated coverage program. |
6. |
Develop proposal and obtain needed agreement by governance/policy boards regarding optimal placement of client/patient billing and collections functions for clients accessing healthcare at SMMC. |
Chronic Disease Management and Care Coordination | |
Overall Goals: | |
● |
Identification and management of patients/members whose complex and/or combination of chronic disease(s) leads to inefficient/ inappropriate utilization of medical resources |
● |
Improved management of chronic disease across systems to ensure efficiency and effectiveness in care coordination and targeting of medical resources |
Key First-Year Actions: | |
1. |
Initiate cross-system chronic disease and care management “champions” who will work with the SMMC Chief Medical Officer and HPSM Medical Director to guide dissemination and improvement of chronic disease management approach. |
2. |
Complete detailed workplan and then launch and disseminate a “Radically Redesigned” model of clinical care that embodies key principles of chronic disease management as well as critical access for patients who would otherwise not be able to utilize care appropriately. |
3. |
Analyze patient/ member statistics and identify target clients to improve assignment of clinical and other resources aimed at improving care and cost management. |
4. |
Initiate mechanisms for continuous/ ongoing monitoring of care statistics to flag areas of focus and resource direction. |
5. |
Develop and implement plan for improving care management of highest cost clients served within SMMC or who “float” between SMMC, HD, HPSM systems to address system issues across continuum of care. |
6. |
Analyze options and develop plans for expanding pilot care coordination initiatives to additional provider setting and/or client populations. |
7. |
Develop plan and implementation schedule for pediatric and geriatric expansions designed around learning in promoting prevention and care coordination. |
Integration Across Levels of Care | |
Overall Goals: | |
● |
Increased proportion of clients being served in most appropriate level setting |
● |
Reduced proportion of clients who do not need acute care being served within an acute care setting |
● |
Improved access and integration across systems for long-term care planning and services |
Key First-Year Actions: | |
1. |
Initiate cross-system workgroup accountable to Health Director and SMMC CEO. |
2. |
Increase sub-acute psychiatric capacity to enable prompt discharge and/or reduced admissions of non-acute psychiatric patients. |
3. |
Develop and implement a plan for increased specialized sub-acute capacity for priority “hard-to-place” patients whose needs are not able to be served by existing acute or sub-acute options that shares risks and responsibilities across systems. |
4. |
Improve assessment of need and diversion of patients presenting at the Emergency Room (ER) and Psychiatric Emergency Services (PES) who are not in need of acute medical care. |
5. |
Develop revised acute admission criteria that better reflect goals and opportunities identified by this workgroup. |
6. |
Analyze current gaps and develop plan to increase Burlingame Long-Term Care (BLTC) capacity to serve clients with behavior challenges. Monitor implementation of plan at the end of six months. |
7. |
Analyze opportunities and develop plan to maximize reimbursement for allowable acute days. Monitor implementation of plan at the end of six months. |
8. |
Standardize philosophy, education and training across systems to achieve increased uniformity and reduced barriers to achieving optimal placement for clients who do not need to be served in an acute care setting. |
9. |
Complete and submit to the State a business and operational plan for the Long-Term Supportive Services Project (LTSSP) to facilitate increased local control and accountability for Medi-Cal long-term care resources. |
10. |
Commission an actuarial study for inclusion of skilled nursing facility (SNF) and adult day health (ADH) funding in HPSM’s capitation rates. |
11. |
Achieve state agreement on rates and plan for inclusion of Medi-Cal SNF and ADH funding within HPSM’s capitation rates. |
12. |
Meet with relevant stakeholders to inform and finalize a start-up and operational plan for LTSSP operations. Initiate actions for LTSSP target start-up date of July 2009, pending successful State negotiations. |
13. |
Assess County’s long-term care needs (e.g., SNF, Assisted Living, housing with on-site supports, other home- and community-based services) in anticipation of LTSSP and local demographic trends. |
Physician Leadership, Relationships and Accountability | |
Overall Goals: | |
● |
Increased alignment of physician leadership and accountability with the healthcare delivery system goals and priorities of SMMC, HPSM and HD |
● |
Improved access and outcomes for patients/members accessing medical care within the County system |
● |
Increased cost-effectiveness in SMMC physician arrangements |
Key First-Year Actions | |
1. |
Create job description and appoint a Chief Medical Officer, with delineated responsibility for physician leadership and accountability distinct from other medical leadership functions in SMMC (e.g., VP of Quality, Department Chairs, other Medical Staff) and HPSM (Medical Director). |
2. |
Develop updated inventory of all employed and contracted physicians to enable analysis and prioritization of opportunities for improved standardization and cost-effectiveness. |
3. |
Determine benchmarks for specialty care access to set employment and contracting standards, expectations and decisions, as well as strategies pursued in developing the Community Health Network for the Underserved. |
4. |
Develop referral standards and guidelines for specialty care services against which access and referrals will be monitored. Develop process for regular monitoring. |
5. |
Develop specific guidelines or models for improving alignment of specialty physicians around chronic disease management. Identify and develop pilot specialties that will serve as models for others. |
6. |
Initiate regular meetings of Chief Medical Officer and key medical and administrative leaders to ensure alignment of clinical philosophy with operational opportunities and constraints, as well as joint identification of areas for priority focus. |
Community Health Network for the Underserved | |
Overall Goal: | |
● |
Creation of a public-private healthcare delivery system for the medically underserved (Medi-Cal and uninsured) that includes defined roles for each major private sector hospital, major ambulatory care providers and a redefined role for SMMC/ the County |
Key First-Year Actions: | |
1. |
Build on provider capacity analysis completed for the BRTF to create an outline, by service area, of provider capacity needed to address the needs of the underserved. |
2. |
Identify, from the deepened provider capacity analysis, targeted roles for each major provider organization that capitalizes on their specific strengths and complements the roles of others to achieve a sustainable distribution of delivery responsibilities across a public/private network. |
3. |
Develop an initial proposal for expanded partnership that targets OB/Pediatrics and achieve agreement from at least three private sector partners. |
4. |
After completing a successful OB/Pediatrics partnership, develop proposals for expanded partnership for each major provider partner and pursue and achieve agreement from each partner. |
5. |
Align scope of services provided by SMMC and to complement partnerships achieved with other providers. |
6. |
Analyze and determine most effective use of unique clinical resources shared across SMMC and the Health Department (Edison Clinic, Mobile Clinics) to best leverage these assets. |
7. |
Consider development of a local “scorecard” that monitors, tracks and publicizes providers’ roles in meeting the needs of the underserved. |
8. |
Communicate private providers’ roles as partners in a new Community Health Network for the Underserved (CHNU) through a County-led media and communications strategy. |
Long-Term Care | |
Overall Goal: | |
● |
Improved County financial position in direct delivery of long-term care services |
Key First-Year Actions: | |
1. |
Assess BLTC to inform County decisions regarding physical plant renovations and/or replacement. |
2. |
Determine point-person for leadership of long-term care business development opportunities within leadership of SMMC, HD, HPSM. |
3. |
Host forum with HMA expert on long-term care business development to discuss potential opportunities and strategies to explore in San Mateo County. |
4. |
Analyze number of skilled nursing facility (SNF) beds that could be guaranteed and paid for by private healthcare providers if capacity were available at SMMC or affiliated sites. |
5. |
Develop several operational and financial models for the operation of SNF services, with guaranteed patients from private healthcare providers. |
6. |
Explore potential management structures/ arrangements to assure efficiency and quality of SNF services. |
7. |
Develop recommendations and obtain agreement on business development targets from appropriate governing boards and private healthcare provider partners. |
Strategic and Operational Financial Improvement | |
Overall Goals: | |
● |
Improved County financial position in delivering medical care |
● |
Improved finance capacity within SMMC to inform strategic health system decisions |
Key First-Year Actions: | |
1. |
Populate SMMC financial decision support system with data and assumptions necessary to develop and refine strategic financial analyses. |
2. |
Identify appropriate financial performance benchmarks and analyze current productivity to select priorities for operational changes. |
3. |
Develop monthly cost and revenue reporting at the service-line, site, specialty, and payer levels. |
4. |
Develop plan for increased Medi-Cal Inter-Governmental Transfer (IGT) to the County (via HPSM) to support SMMC operations. |
5. |
Develop and implement plan to improve billing and collections functions. |
6. |
Analyze opportunities to restructure current debt service. |
Next Steps | |
In addition to carrying out the implementation activities detailed above, the Redesign team is committed to keeping stakeholders informed of progress in meeting key milestones. Team members have developed a communication plan that includes updates to the relevant governing boards and the Board of Supervisors, including an update to the Board of Supervisors in September 2008 on the first six months of the Redesign effort. The Redesign team will also post key communications on the website developed for the BRTF and expects to reconvene interested task force members during the first quarter of 2009 to report back to these community partners on the Redesign Initiative. | |
The Redesign Team will also be overseeing an external evaluation of the Redesign effort that will include a locally tailored review of the “Coverage Initiative”, supported by State and Federal Medicaid funding that represents a pilot of the BRTF preliminary recommendations, as well as systems integration efforts targeted by the Redesign Initiative. This evaluation will include an assessment of the overall impact of the Redesign effort on issues of priority concern, such as access to healthcare across our systems and effective use of our local healthcare resources and assets. | |